Defining Positive Support
The term Positive Support refers to strategies and practices that are:
- Person-centered in nature, sensitive to the unique cultures and backgrounds of each individual, and respectful towards people receiving these supports;
- Evidence-based or promising practices;
- Adapted and improved over time using assessment processes to guide use; and
- Often implemented with more than one evidence-based or promising practices as part of a team-based approach.
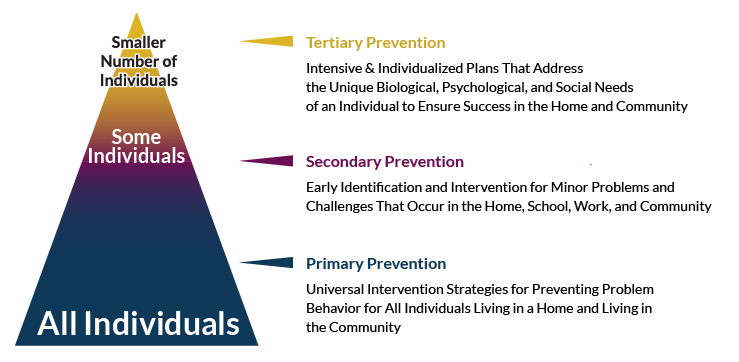
One way to think about positive support practices is to consider it from a public health disease prevention model used by the World Health Organization. The figure below describes how this model addresses the prevention of mental health related issues and the occurrence of problem behavior across three levels by improving quality of life.
When a vision that is articulated by a group of people is made a part of everyday actions taken within an organization, county, region, and state-wide, significant and meaningful work can be achieved. —Fullan, 2005
Examples of Positive Supports
- Applied Behavior Analysis
- Cognitive Behavior Therapy
- Dialectical Behavior Therapy
- Person-centered Thinking and Planning
- Positive Behavior Support
- Systems of Care
- Wraparound Planning
- Trauma Informed Practices
- Multisystemic Therapy
- Response to Intervention
Primary Prevention includes universal strategies for supporting all individuals in a home or community. The goal at the Primary Prevention level is to implement strategies for social and behavioral health across all persons. Secondary Prevention includes early identification of problems that may be occurring with simple strategies for addressing social behavior or mental health issues. Interventions at the Tertiary Prevention Level are used to address chronic and severe problem behaviors or mental illness. Positive support practices used in organizations address different prevention levels. Multiple positive support practices may be needed to prevent mental illness or problematic behavior.
Public Health Model for Preventing Problem Behavior
The Biological-Psychological-Social Model
Biological, psychological, and social factors can impact a person’s behavior. For this reason, strategies from a variety of fields are used by a person and his team as part of a problem-solving process. Teams use research from developmental disabilities, mental health, social work, aging, and traumatic brain injury to support a person and her family. The practices identified are based on that person’s unique biological, psychological, and social characteristics.
The Biological, psychological, social (biopsychosocial) approach provides a framework that includes the interacting components from these three domains, in both the assessment and treatment of medical and behavioral issues. Including all three domains in assessment and treatment acknowledges the importance of holistic approaches to successfully treating people with severe issues. While the approach was originally developed by medical practitioners for identifying the multiple causes of severe medical issues, it is equally effective for assessing and treating severe behavioral issues.
We are all concerned about improving clinical outcomes, treating aggression and self-injurious behavior, reducing cost of care, decreasing the use of restraints and seclusion, and improving the quality of life for people who use services and people who provide services. These outcomes can be achieved more readily using precise treatments and supports that are designed one person at a time and based on the specific variables that trigger and maintain aggression or self-injury, which often vary person by person. The bio-psycho-social model offers a methodology for systematically identifying which biological, psychological, and/or social variables contribute to episodes of self-injury or aggression; identifying also illuminates possible treatment strategies.

